AI in mental health care: Bridging the gap
Nearly everyone knows someone living with a mental health condition - whether it's depression, anxiety, or PTSD. According to NHS England, one in four adults will experience a diagnosable mental health condition each year, yet fewer than half receive the treatment they need. This widening gap between those needing help and those receiving it creates an urgent need for innovative solutions.
So how AI can make mental healthcare more accessible, personalized, and effective?
Behind every mental health statistic is a real person - someone waiting for therapy, struggling with anxiety, or battling depression without adequate support.
Traditional mental healthcare systems were already stretched thin before the pandemic, and now they're facing unprecedented demand they simply cannot meet.
This is where AI offers something different - not as a replacement for human therapists, but as a critical bridge to provide immediate, personalized, and accessible support when traditional services fall short.
The human cost of mental healthcare gaps
In the UK and US, millions of people are on waiting lists for mental health support, while many others cannot access care due to cost, location, or provider shortages. These aren't just statistics - each represents a person experiencing real suffering, from teenagers with anxiety to workers struggling with depression to older adults facing isolation.
The cost is enormous - both in human suffering and economic impact. The personal toll is even more devastating, with untreated mental health issues leading to worsening physical health, broken relationships, and in worst cases, loss of life.
Next-generation mental health companions
Today's AI mental health solutions offer sophisticated support designed to address specific gaps in care:
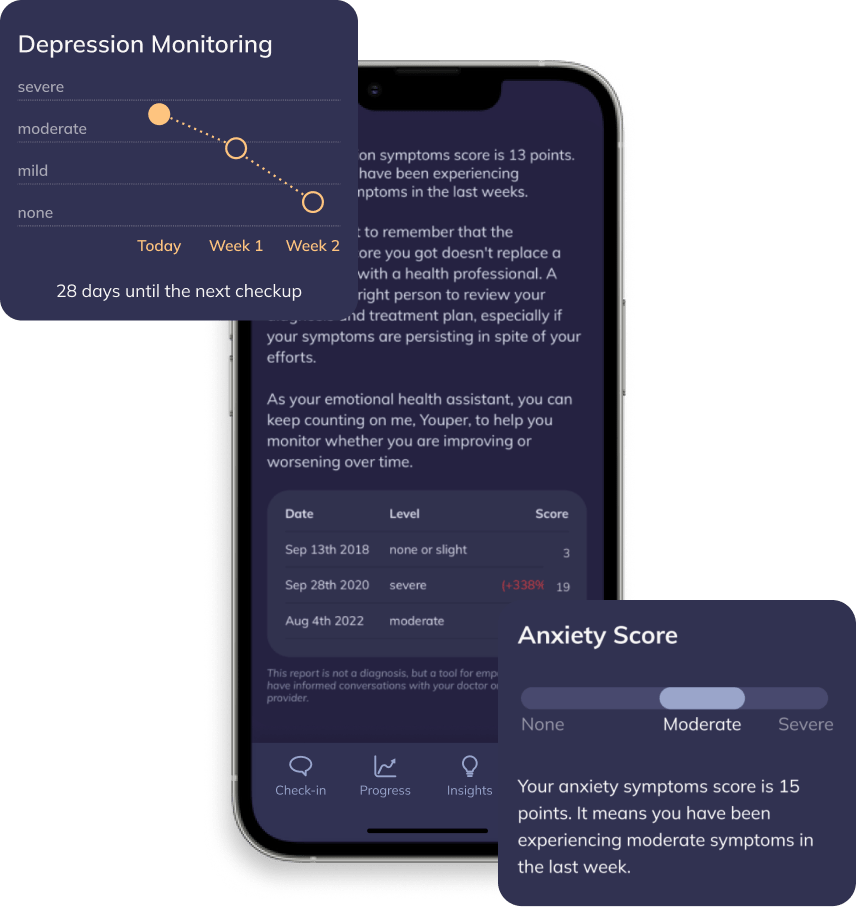
Youper, an AI-powered mental health app, uses evidence-based techniques like cognitive behavioral therapy (CBT) for personalized support. The app offers guided conversations, mood tracking, and self-reflection exercises to help manage anxiety, depression, and stress. Stanford University research has validated its effectiveness - over 80% of millions of users report improved well-being from using this privacy-focused, adaptive chatbot.
Cass, a psychologist-developed AI-enabled mental health chatbot, provides round-the-clock support through evidence-based therapeutic approaches like CBT. This clinically proven platform delivers personalized, context-aware conversations that have shown measurable reductions in users' depression and anxiety symptoms.
Earkick combines AI with real-time biometric tracking to deliver personalized mental health interventions. Their wearable monitors physiological signs of stress, while the AI companion offers context-aware coping strategies.
Wysa combines AI self-help with human coaching in a stepped-care approach: users begin with an AI chatbot for immediate support and can connect with licensed therapists when needed.
Condition-specific AI interventions
More targeted solutions are emerging for specific mental health conditions:
NOCD delivers AI-supported exposure and response prevention (ERP) therapy for obsessive-compulsive disorder (OCD). This platform combines self-guided digital exercises with video therapy sessions, making a specialized treatment accessible to people who might otherwise wait months to see an OCD specialist.
Researchers at Dartmouth have developed Therabot, a conversational AI designed specifically for people on treatment waiting lists. A recent study of 106 participants found that patients with depression experienced a 51% average reduction in symptoms, leading to significant clinical improvements in mood and overall well-being. Those with generalized anxiety showed an average 31% reduction in symptoms, with many participants moving from moderate to mild anxiety levels, or dropping below the clinical threshold for diagnosis.
“We did not expect that people would almost treat the software like a friend. It says to me that they were actually forming relationships with Therabot.”
Neurofit is a neuroscience-based wellness app that uses AI to deliver personalized somatic exercises, daily check-ins, and real-time biometric feedback to help users regulate their nervous system and reduce chronic stress. Active members report an average 54% reduction in stress after just one week, with AI-guided coaching and integration with wearables like Apple Watch for tailored stress management and emotional support.
What's actually working?
The most promising AI mental health tools share several characteristics:
Evidence-based foundations: They incorporate established therapeutic approaches like CBT, acceptance and commitment therapy (ACT), or mindfulness.
Clear scope and limitations: Responsible tools are transparent about what they can and cannot do, with appropriate safety measures for crisis situations.
Ongoing validation: Leading companies conduct and publish research on their platforms' effectiveness.
Human-in-the-loop design: The most effective solutions maintain some level of human oversight or escalation pathways.
Privacy-first approach: Given the sensitive nature of mental health data, robust privacy protections are non-negotiable.
The road ahead: Challenges and opportunities
As promising as these technologies are, significant challenges remain:
Regulatory uncertainty: The regulatory landscape for AI mental health tools remains fragmented, creating both opportunities for innovation and risks for consumers.
Data privacy concerns: Mental health data is exceptionally sensitive. Companies must navigate complex privacy regulations while collecting enough data to improve their algorithms.
Equity and access: While AI tools can theoretically improve access to mental health support, there's a risk of exacerbating existing inequities if they require resources not equally available across populations.
Integration with traditional care: The most effective future isn't standalone AI solutions but integration with traditional care systems, where AI tools provide initial support with seamless escalation to human providers when needed.
One of the most prominent mental health chatbots, Woebot, recently announced it will shut down its signature app on June 30. The AI-powered tool, developed by clinical psychologists used cognitive-behavioral therapy (CBT) principles to provide users with daily conversational support, practical coping strategies, and mood tracking to help manage anxiety, depression, and stress.
🔮 Looking ahead
In the next 3 years, expect more clinically validated tools with specific therapeutic focuses and increased integration with wearables for personalized interventions.
In 5 years, AI tools will likely become standard components of mental healthcare delivery, with clearer regulatory frameworks and improved natural language processing capabilities.
Within a decade, truly personalized mental health AI could emerge - systems that adapt not just to symptoms but to personality, communication style, and therapeutic preferences, potentially identifying mental health risks before symptoms appear.
A balanced perspective
AI cannot replace the empathy, intuition, and human connection that are fundamental to therapeutic relationships. What it can provide is a valuable bridge - support when nothing else is available, a stepping stone to human care, or a complement to traditional therapy.
The key question isn't whether AI can perfectly replicate human therapy - it's whether it can help reduce suffering for those who would otherwise receive no care at all. For many people, early evidence suggests it can make a meaningful difference.
📫 Subscribe to the Healthy Innovations newsletter for your weekly dose of medical advances, from AI diagnostics to gene therapies, delivered in a concise 5-minute read.