GLP-1: From diabetes drug to healthcare revolution
“We tend to think of drugs as surgically designed to do only one thing.
But the reality is almost never like this.”
Beyond glucose control: The multisystem impact of GLP-1 therapy
What began as a treatment for type 2 diabetes (T2D) has evolved into something far more significant – potentially one of the most versatile therapeutic classes in modern medicine.
GLP-1 receptor agonists work by mimicking a naturally occurring hormone, but their clinical effects reach well beyond blood sugar regulation. These medications are creating a major shift in how we approach multiple chronic diseases.
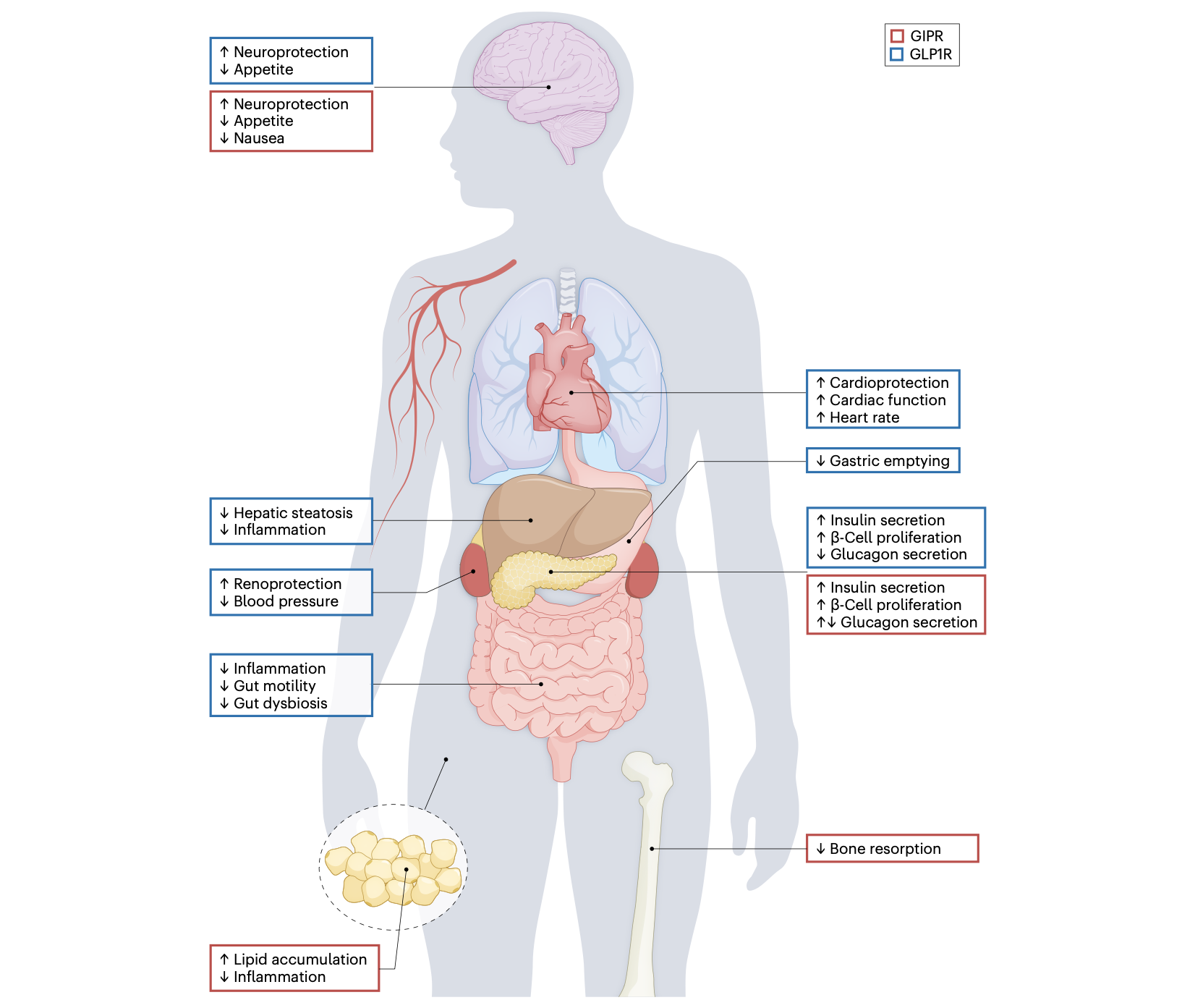
The secret to their wide-ranging benefits lies in the distribution of GLP-1 receptors throughout the body. These receptors aren't just found in the pancreas - they're expressed in the brain, heart, kidneys, blood vessels, immune cells, and gastrointestinal tract. This widespread presence creates a biological network through which a single medication class can address multiple interconnected conditions.
GLP-1 is part of a family of incretin hormones that also includes GIP (Glucose-dependent Insulinotropic Polypeptide). While GLP-1 has received more attention, GIP also plays important roles in metabolism, bone health, and inflammation. GIP receptors are distributed throughout the body in adipose tissue, bone, the immune system, and the central nervous system. The therapeutic exploitation of both GLP-1 and GIP pathways is now yielding exciting new treatment possibilities.
Cardiovascular protection: GLP-1 receptors in cardiac tissue and blood vessels help reduce inflammation, improve endothelial function, and potentially stabilize atherosclerotic plaques. Major cardiovascular outcome trials with liraglutide, semaglutide, and dulaglutide have consistently demonstrated reductions in heart attacks, strokes, and cardiovascular deaths - benefits that extend even to patients with obesity who don't have diabetes.
Inflammation control: Perhaps the most significant mechanism underlying GLP-1's diverse benefits is its powerful anti-inflammatory effect. These medications reduce pro-inflammatory cytokines, decrease macrophage activation, and improve vascular endothelial function across multiple organ systems. GLP-1 receptors expressed on intestinal intraepithelial lymphocytes help regulate microbiome-dependent inflammation, contributing to broader systemic anti-inflammatory effects.
Kidney protection: GLP-1 receptors located specifically in the smooth muscle cells of kidney afferent arterioles help enhance sodium and water excretion while reducing albumin excretion. Clinical trials show these medications can meaningfully slow the progression of chronic kidney disease in people with T2D. Post-hoc analyses have demonstrated modest but significant reductions in the rate of kidney function decline, particularly benefiting those with already reduced kidney function.
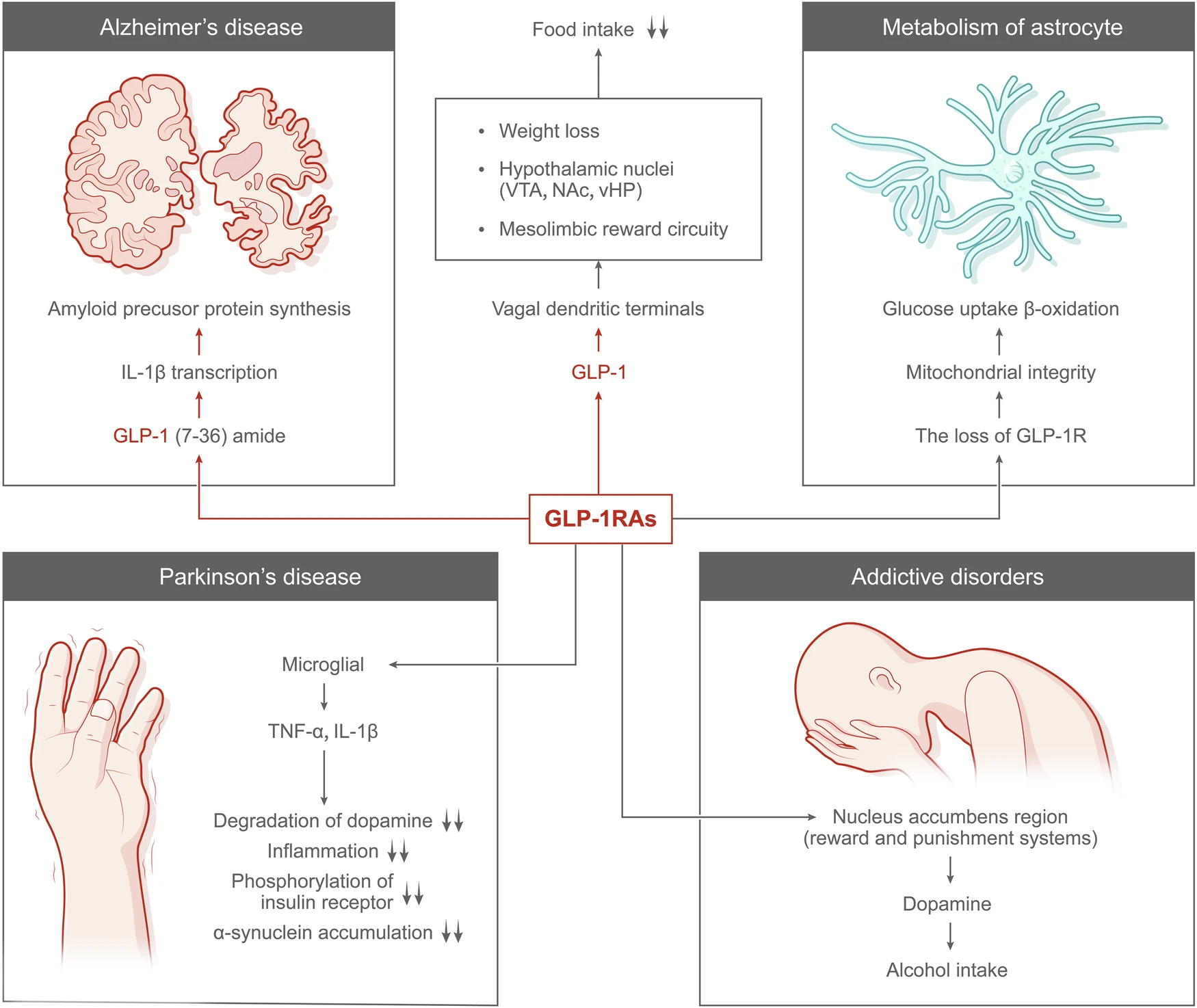
Brain health: The neuroprotective actions of GLP-1s include enhanced neuronal proliferation and survival, reduced oxidative stress, decreased neuroinflammation, and improved blood-brain barrier function. Small clinical trials examining exenatide in Parkinson's disease patients have shown improved motor function that persisted even after stopping the medication. Meanwhile, large trials are underway to investigate their potential in preventing cognitive decline and Alzheimer's disease.
Liver restoration: GLP-1s have proven remarkably effective at reducing liver fat accumulation, with some patients experiencing complete resolution of non-alcoholic steatohepatitis (NASH). This has prompted phase III clinical trials of semaglutide specifically for treating this serious liver condition.
Most intriguingly, many of these benefits appear to be independent of weight loss. Even in patients who don't lose significant weight, GLP-1s demonstrate organ protection across multiple systems, suggesting direct effects that transcend their impact on body weight.
Reimagining chronic disease care
This convergence of benefits is forcing us to rethink our siloed approach to chronic disease. Rather than treating each condition separately - diabetes with one medication, cardiovascular disease with another, kidney problems with a third - GLP-1 therapy suggests an integrated approach that recognizes the interconnected nature of metabolic, cardiovascular, renal, and neurological health.
For clinicians, GLP-1s blur the lines between medical specialties. Should these medications be prescribed by endocrinologists, cardiologists, nephrologists, or primary care physicians? The answer increasingly seems to be "all of the above," suggesting a more integrated, patient-centered approach to chronic disease management.
For healthcare systems, GLP-1s present both challenges and opportunities. Their high cost creates short-term financial pressure, but their ability to prevent costly complications across multiple organ systems may ultimately reduce long-term healthcare expenditures.
The road ahead: Challenges and opportunities
Despite their promise, several critical challenges remain:
Access and affordability: The high cost of these medications creates significant access barriers. While pharmaceutical companies have initiated some patient assistance programs, broader policy solutions are needed to ensure equitable access.
Long-term safety data: While short-term safety profiles appear generally favorable, questions remain about potential rare side effects with long-term use, especially as these medications expand to new populations.
Societal implications: As GLP-1s become more widely used for obesity, important questions arise about the medicalization of body weight and the intersection of medical treatment with societal attitudes toward body size and health.
Differential tissue benefits: Current GLP-1 receptor agonists may not uniformly affect all tissues where the receptor is expressed. For example, while liraglutide significantly improves glycemic control and cardiovascular outcomes, its effects on bone density are less clear despite GLP-1 receptors being present in bone tissue. Similarly, GIP has direct actions on bone, immune cells, and fat metabolism that differ from GLP-1's effects. Understanding these tissue-specific responses will be crucial for developing more targeted therapies.
Looking forward
What might the future hold for GLP-1 receptor agonists and related incretin therapies?
In the next 3-5 years, we can expect expanded indications for existing GLP-1s beyond diabetes and obesity, particularly for heart failure, chronic kidney disease, and fatty liver disease. Improved formulations will likely reduce gastrointestinal side effects and possibly extend the dosing interval from weekly to monthly.
Looking 5-10 years ahead, oral formulations may become more widely available, addressing the current limitation of injection-only delivery for most GLP-1 therapies. We're also likely to see more sophisticated targeting of specific GLP-1 receptor signaling pathways, potentially separating the beneficial metabolic effects from unwanted side effects.
The next decade will also likely bring further development of multi-agonist drugs beyond tirzepatide, aiming to mimic the complex hormonal changes seen after bariatric surgery to maximize therapeutic benefits across multiple metabolic pathways.
Perhaps most exciting is the potential for GLP-1s to revolutionize our approach to chronic disease prevention. These medications may meaningfully reduce the risk of diabetes, heart disease, kidney failure, and possibly neurodegenerative conditions - shifting healthcare's focus from treatment to prevention.
The GLP-1 revolution transcends being just another medication class. It challenges our fundamental understanding of chronic diseases as isolated conditions, instead revealing an integrated view where metabolic, cardiovascular, kidney, and brain health are deeply interconnected.
For healthcare providers, researchers, and patients alike, this offers a powerful new perspective on human health and disease. The question isn't whether GLP-1s will transform medicine - they already are. The real question is how fully we'll embrace their paradigm shift toward integrated, preventative care.
📫 Subscribe to the Healthy Innovations newsletter for your weekly dose of medical advances, from AI diagnostics to gene therapies, delivered in a concise 5-minute read.